Dysautonomia
When the Body’s Automatic Systems Don’t Feel Automatic
Do you ever feel dizzy when standing up, lightheaded after meals, or constantly tired without understanding why? These can be signs of dysautonomia — a condition where the autonomic nervous system (ANS), which controls automatic body functions like heart rate, blood pressure, and digestion, isn’t regulating properly.
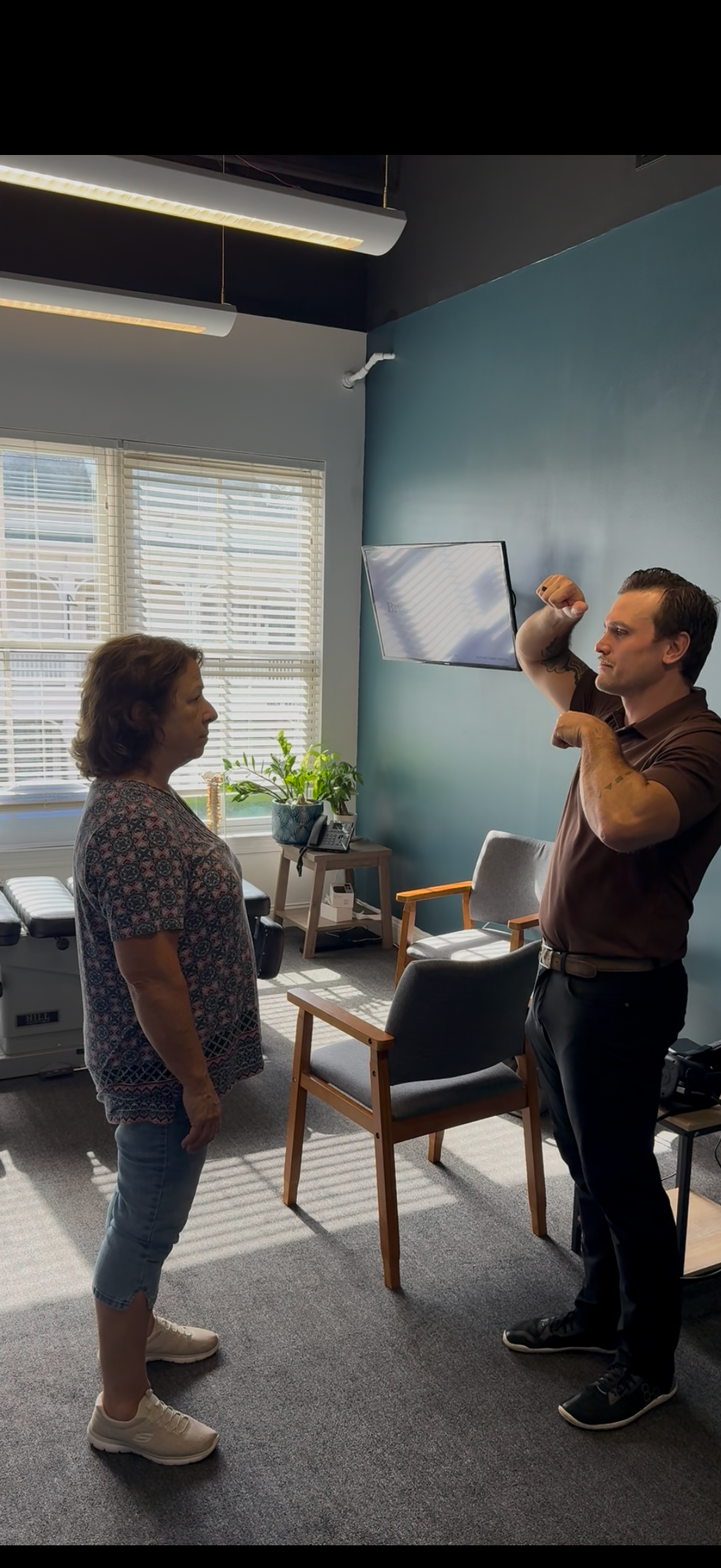
At SCC Neuro, we help patients find real explanations — and real progress — through neurological assessment and neurorehabilitation designed to restore balance to the autonomic nervous system.
What Is Dysautonomia?
The autonomic nervous system (ANS) controls things you don’t have to think about — breathing, heart rate, temperature, blood pressure, and digestion.
When it doesn’t function properly, you might experience:
Dizziness or fainting when standing
Rapid heartbeat or palpitations
Brain fog or lightheadedness
Temperature sensitivity
Fatigue or exercise intolerance
Anxiety-like symptoms without emotional cause
These symptoms are your body’s way of saying the neural circuits regulating balance and circulation are out of sync.
Types of Dysautonomia We See
There are several forms, but we often help patients with:
Postural Orthostatic Tachycardia Syndrome (POTS)
Neurocardiogenic Syncope (NCS)
Orthostatic Intolerance
Vasovagal Episodes
Autonomic instability following concussion or infection
The Brain–Body Connection
Your autonomic nervous system is controlled by the brainstem, cerebellum, and higher cortical centers.
If communication between these regions becomes unbalanced due to injury, inflammation, or chronic stress, the result can be unpredictable regulation of blood pressure, heart rate, and sensory responses.
At SCC Neuro, we identify where the disconnect is occurring — and retrain those circuits to function normally again.
Functional Neurology Evaluation
Your evaluation may include:
Assessment of heart rate and blood pressure changes
Vestibular and balance testing
Eye movement and brainstem reflex analysis
Autonomic response testing (autonomics, pupillometry)
Cerebellar and cortical function evaluation
This helps map how your brain communicates with your body’s automatic systems.
Neurorehabilitation for Dysautonomia
Treatment is personalized and gentle, focusing on stabilizing the autonomic network while improving resilience.
Common therapies include:
Autonomic regulation training and graded movement rehab
Visual-vestibular integration to stabilize circulation control reflexes
Balance and cerebellar coordination therapy
Breathing and parasympathetic activation exercises
Sensory input and neurofeedback retraining
Our goal: help your body self-regulate again — without needing to fight through symptoms.
Take the First Step Toward Balance
You don’t have to keep “pushing through” dysautonomia. Through individualized neurological care, we’ll help you rebuild the foundations of your body’s regulation and resilience.
Functional Neurological Evaluation and Rehabilitation for Dysautonomia
Dysautonomia encompasses a range of conditions characterized by functional disturbances in the autonomic nervous system (ANS), leading to inappropriate cardiovascular, respiratory, and thermoregulatory responses. At SCC Neuro, we approach dysautonomia through a functional neuroscience framework, emphasizing restoration of autonomic network integrity within the brainstem, cerebellar, and cortical systems.
Pathophysiology
The autonomic nervous system maintains homeostasis via reciprocal sympathetic and parasympathetic regulation.
Dysautonomia arises from:
Brainstem dysregulation impacting baroreceptor or vagal tone
Cerebellar or cortical involvement altering integration of autonomic reflexes
Altered vestibulo-autonomic coupling after concussion or sensory mismatch
Neuroimmune or metabolic mechanisms disrupting autonomic feedback pathways
These dysfunctions create inconsistent neurovascular control, producing symptoms such as orthostatic tachycardia, syncope, temperature dysregulation, and cognitive fatigue.
Clinical Presentation
Patients commonly present with:
Reduced joint stability or endurance under load
Altered coordination and delayed muscle activation timing
Persistent pain despite normal imaging findings
Impairment of balance or fine motor control
Secondary headaches or neck discomfort from compensatory strain
Such findings indicate neural maladaptation beyond localized soft tissue injury.
Clinical Manifestations
Patients with dysautonomia may present with:
Orthostatic intolerance or postural tachycardia (POTS)
Syncope or near-syncope with minimal exertion
Fluctuating blood pressure and heart rate variability
Cognitive fog and mental fatigue
Sensory hypersensitivity (light, noise, or motion)
Altered temperature, sweating, or GI motility regulation
Autonomic symptoms often coexist with vestibular or cerebellar dysfunction following mild traumatic brain injury or systemic illness.
Functional Neurological Evaluation
Clinical evaluation integrates:
Quantitative heart rate variability (HRV) and baroreflex analysis
Pupillometry and ocular control testing for central autonomic function
Vestibular-autonomic reflex assessment
Hemispheric and cerebellar activation mapping
Dynamic posturography and orthostatic testing
This model identifies regional dysfunction within the central-autonomic network to guide precise neurorehabilitative intervention.
Rehabilitation Strategy
Neurorehabilitation protocols focus on improving cerebro-autonomic integration and resilience under graded sensory and postural demand:
Gradual orthostatic adaptation through dynamic positional retraining
Cerebellar activation protocols for autonomic modulation
Breathing and vagal tone retraining to enhance parasympathetic dominance
Visual-vestibular integration to normalize autonomic reactivity
Low-intensity neuro-motor and balance-based reconditioning
Therapeutic dosing is patient-specific and responsive to HRV, dizziness provocation, and autonomic load tolerance.
Clinical Goals
Functional outcomes include:
Enhanced autonomic stability and cardiovascular control
Improved cognitive endurance and orthostatic tolerance
Normalized HRV and baroreflex sensitivity
Reduction in symptom provocation with daily activity
Increased parasympathetic resilience and systemic regulation
Why SCC Neuro
Postgraduate training in Clinical Neuroscience and Autonomic Rehabilitation
Advanced diagnostic and biofeedback technologies
Integration of functional neurology with evidence-based rehabilitative neuroscience
Collaborative approach to care for complex autonomic disorders
Professional Consultation and Referral
Dysautonomia frequently follows concussion, infection, or systemic inflammation and benefits from interdisciplinary management.
Clinicians seeking collaborative management or referral for complex autonomic dysfunction are welcome to contact SCC Neuro for advanced functional-neurology assessments and targeted care.